Rev
Bras
Anestesiol.
2019;69(2):168---176
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Publicação
Oficial
da
Sociedade
Brasileira
de
Anestesiologia
www.sba.com.br
SCIENTIFIC
ARTICLE
YouTube
as
an
informational
source
for
brachial
plexus
blocks:
evaluation
of
content
and
educational
value
Onur
Selvi
a
,∗
,
Serkan
Tulgar
a
,
Ozgur
Senturk
a
,
Deniz
I.
Topcu
b
,
Zeliha
Ozer
a
a
Maltepe
University,
Faculty
of
Medicine,
Department
of
Anesthesiology
and
Reanimation,
Istanbul,
Turkey
b
Gazi
University,
Institute
of
Health
Sciences,
Department
of
Medical
Biochemistry,
Ankara,
Turkey
Received
30
March
2018;
accepted
5
November
2018
Available
online
21
December
2018
KEYWORDS
YouTube;
Anesthesia;
Brachial
plexus
blocks
Abstract
Background
and
objectives: YouTube,
the
most
popular
video-sharing
website,
contains
a
signif-
icant
number
of
medical
videos
including
brachial
plexus
nerve
blocks.
Despite
the
widespread
use
of
this
platform
as
a
medical
information
source,
there
is
no
regulation
for
the
quality
or
content
of
the
videos.
The
goals
of
this
study
are
to
evaluate
the
content
of
material
on
YouTube
relevant
to
performance
of
brachial
plexus
nerve
blocks
and
its
quality
as
a
visual
digital
information
source.
Methods:
The
YouTube
search
was
performed
using
keywords
associated
with
brachial
plexus
nerve
blocks
and
the
final
86
videos
out
of
374
were
included
in
the
watch
list.
The
asses-
sors
scored
the
videos
separately
according
to
the
Questionnaires.
Questionnaire-1
(Q1)
was
prepared
according
to
the
ASRA
guidelines/Miller’s
Anesthesia
as
a
reference
text
book,
and
Questionnaire-2
(Q2)
was
formulated
using
a
modification
of
the
criteria
in
Evaluation
of
Video
Media
Guidelines.
Results:
72
ultrasound-guided
and
14
nerve-stimulator
guided
block
videos
were
evaluated.
In
Q1,
for
ultrasound-guided
videos,
the
least
scores
were
for
Q 1 --- 5
(1.38)
regarding
the
complications,
and
the
greatest
scores
were
for
Q1---13
(3.30)
regarding
the
sono-anatomic
image.
In
videos
with
nerve
stimulator,
the
lowest
and
the
highest
scores
were
given
for
Q 1 --- 7
(1.64)
regarding
the
equipment
and
Q1---12
(3.60)
regarding
the
explanation
of
muscle
twitches
respectively.
In
Q2,
65.3%
of
ultrasound-guided
and
42.8%
of
blocks
with
nerve-stimulator
had
worse
than
satisfactory
scores.
Conclusions:
The
majority
of
the
videos
examined
for
this
study
lack
the
comprehensive
approach
necessary
to
safely
guide
someone
seeking
information
about
brachial
plexus
nerve
blocks.
©
2018
Published
by
Elsevier
Editora
Ltda.
on
behalf
of
Sociedade
Brasileira
de
Anestesiologia.
This
is
an
open
access
article
under
the
CC
BY-NC-ND
license
(http://creativecommons.org/
licenses/by-nc-nd/4.0/
).
∗
Corresponding
author.
E-mail:
(O.
Selvi).
https://doi.org/10.1016/j.bjane.2018.12.005
0104-0014/©
2018
Published
by
Elsevier
Editora
Ltda.
on
behalf
of
Sociedade
Brasileira
de
Anestesiologia.
This
is
an
open
access
article
under
the
CC
BY-NC-ND
license
(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Brachial
plexus
videos
in
YouTube
169
PALAVRAS-CHAVE
YouTube;
Anestesia;
Bloqueios
do
plexo
braquial
YouTube
como
fonte
informativa
sobre
bloqueios
do
plexo
braquial:
avaliac¸ão
de
conteúdo
e
valor
educativo
Resumo
Justificativa
e
objetivos:
O
YouTube,
site
de
compartilhamento
de
vídeos
mais
popular,
contém
um
número
significativo
de
vídeos
médicos,
incluindo
bloqueios
do
plexo
braquial.
Apesar
do
uso
generalizado
dessa
plataforma
como
fonte
de
informac¸ão
médica,
não
há
regulamentac¸ão
para
a
qualidade
ou
o
conteúdo
dos
vídeos.
O
objetivo
deste
estudo
é
avaliar
o
conteúdo
do
material
no
YouTube
relevante
para
o
desempenho
do
bloqueio
do
plexo
braquial
e
sua
qualidade
como
fonte
de
informac¸ão
visual
digital.
Métodos:
A
pesquisa
no
YouTube
foi
realizada
usando
palavras-chave
associadas
ao
bloqueio
do
plexo
braquial
e,
de
374
vídeos,
86
foram
incluídos
na
lista
de
observac¸ão.
Os
avaliadores
classificaram
os
vídeos
separadamente,
de
acordo
com
os
questionários.
O
questionário-1
(Q1)
foi
preparado
de
acordo
com
as
diretrizes
da
ASRA/Miller’s
Anesthesia
como
livro
de
referência
e
o
Questionário-2
(Q2)
foi
formulado
usando
uma
modificac¸ão
dos
critérios
em
Avaliac¸ão
de
Diretrizes
para
Mídia
de
Vídeo.
Resultados:
No
total,
72
vídeos
sobre
bloqueios
guiados
por
ultrassom
e
14
vídeos
sobre
bloqueios
com
estimulador
de
nervos
foram
avaliados.
No
Q1,
para
os
vídeos
apresen-
tando
bloqueios
guiados
por
ultrassom,
os
menores
escores
foram
para
Q 1 --- 5
(1,38)
em
relac¸ão
às
complicac¸ões
e
os
maiores
escores
foram
para
Q1---13
(3,30)
em
relac¸ão
à
imagem
sonoanatômica.
Nos
vídeos
que
apresentaram
bloqueios
com
estimulador
de
nervos,
os
menores
e
os
maiores
escores
foram
dados
para
Q 1 --- 7
(1,64)
em
relac¸ão
ao
equipamento
e
Q1---12
(3,60)
em
relac¸ão
à
explicac¸ão
das
contrac¸ões
musculares,
respectivamente.
No
Q2,
65,3%
dos
blo-
queios
guiados
por
ultrassom
e
42,8%
dos
bloqueios
com
estimulador
de
nervos
apresentaram
escores
abaixo
de
satisfatórios.
Conclusões:
A
maioria
dos
vídeos
examinados
para
este
estudo
carece
da
abordagem
abrangente
necessária
para
orientar
com
seguranc¸a
as
pessoas
que
buscam
informac¸ões
sobre
o
bloqueio
do
plexo
braquial.
©
2018
Publicado
por
Elsevier
Editora
Ltda.
em
nome
de
Sociedade
Brasileira
de
Anestesiologia.
Este
´
e
um
artigo
Open
Access
sob
uma
licenc¸a
CC
BY-NC-ND
(http://creativecommons.org/
licenses/by-nc-nd/4.0/
).
Introduction
YouTube
(YouTube
©
www.youtube.com,
YouTubeLLC,
San
Bruno,
USA)
as
a
referential
visual
guide
is
one
of
the
most
popular
digital
information
sources
currently
available,
with
more
than
4
billion
videos
watched
every
day.
The
health-
care
social
media
listings
of
the
Mayo
Clinic
name
>700
health-related
organizations
in
the
United
States
of
Amer-
ica
alone
that
have
a
presence
on
YouTube.
Some
of
the
videos
were
prepared
for
healthcare
providers
as
an
educa-
tional
visual
guide
for
new
interventions.
1
However,
there
are
no
regulations
or
standards
with
respect
to
the
educa-
tional
aspects
of
the
videos
available
on
YouTube.
Misleading
information
has
been
shared
on
YouTube
which
could
pose
risk
to
healthcare
professionals
or
their
patients.
2
On
the
other
hand,
E-Learning
methods
such
as
video
recordings
have
become
an
important
part
of
medical
education.
3 --- 6
It
has
been
proven
in
many
studies
that
learning
through
visual
sources
has
many
advantages
over
conventional
didac-
tic
training
methods
for
both
medical
students
and
in
other
areas
of
medical
training
including
regional
anesthesia.
7
Especially,
in
regional
anesthesiology
education
and
training,
there
is
value
in
offering
clear
visual
guidance
to
clarify
the
complex
interactions
of
anatomy,
manual
skills,
physiology,
and
clinical
judgment.
Several
regional
anesthesia
institutions
regularly
publish
comprehensive
educational
multimedia
materials
for
such
advanced
inter-
ventions
however;
such
proprietary
materials
may
not
achieve
the
dissemination
impact
of
YouTube.
Increas-
ingly,
YouTube
is
being
recognized
as
a
potentially
useful
source
of
healthcare
education
and
training
material.
8
On
YouTube
one
may
easily
reach
information
on
a
complex
idea
relayed
through
a
basic
visual
format.
However,
it
is
currently
possible
for
accurate
information
to
be
displayed
on
YouTube
in
a
way
that
is
disorganized,
disjointed
or
even
misleading.
1
Until
today,
videos
of
neuroxial
block
techniques
and
lumbar
punctures
on
YouTube
have
been
assessed
regarding
patient
safety,
consistency
with
a
scientific
approach,
and
their
quality.
9,10
The
aim
of
this
study
was
to
evaluate
YouTube
videos
relevant
to
performance
and
preparation
of
brachial
plexus
nerve
blocks,
using
ASRA
guidelines
and
Miller’s
Anesthesia
as
reference
texts.
11,12
Methods
Video
selection
BPNB
procedures
were
selected
as
the
target
group
for
the
YouTube
videos
to
be
evaluated
with
the
concensus

170
O.
Selvi
et
al.
from
the
authors.
The
YouTube
search
for
videos
of
axil-
lary,
infraclavicular,
interscalene
and
supraclavicular
nerve
blocks,
which
are
extensively
used
for
shoulder,
arm
and
hand
surgeries,
was
completed
on
06.10.2017
by
the
main
investigator,
an
anesthesiologist
with
8
years
experience
in
anesthesia.
The
selected
keywords
were
‘‘interscalene
block
ultrasound’’,
‘‘interscalene
block
nerve
stimulator’’,
‘‘supraclavicular
block
ultrasound’’,
‘‘supraclavicular
block
nerve
stimulator’’,
‘‘infraclavicular
block
ultrasound’’,
‘‘infraclavicular
block
nerve
stimulator’’,
‘‘axillary
block
ultrasound’’,
‘‘axillary
block
nerve
stimulator’’.
Establishment
of
assessor
team
One
consultant
anesthesiologist
and
three
experienced
anesthesiologists
with
more
than
7
years’
experience
in
anesthesia
were
selected
as
the
assessor
team.
All
of
them
can
safely
practice
the
blocks
mentioned
above
in
their
daily
routine
and
also
teach
them
as
part
of
a
trainee
education
program.
Tw o
of
them
had
of
Turkish
Regional
Anesthe-
sia
Society
ultrasound
guided
regional
anesthesia
training
certificates.
The
main
investigator,
as
team
leader,
orga-
nized
a
work
shop.
In
this
workshop
random
lower
extremity
regional
anesthesia
videos
were
selected
from
YouTube
and
assessors
were
asked
to
score
the
videos
in
a
form
which
was
specifically
prepared
for
data
entry.
Information
gathered
during
the
workshop
was
used
to
determine
any
ambiguous
points
about
data
recording,
scoring
system
and
exclusion
criteria,
leading
to
clarification
of
the
study
objectives.
Any
disputed
topics
related
to
these
elements
were
determined
through
consensus.
Watch
list
The
main
investigator
prescreened
the
first
100
recent
and
popular
videos
to
create
a
‘‘watch
list’’
regarding
each
key-
word
while
further
pages
were
not
included
in
the
search
due
to
the
frequency
of
obsolete,
irrelevant
or
repeated
material.
The
search
was
limited
to
the
first
100
videos
as
it
was
not
the
aim
of
the
investigators
to
evaluate
all
videos,
but
only
those
which
would
have
the
highest
possi-
bility
of
being
viewed.
Due
to
the
YouTube
search
algorithm,
results
of
the
search
were
listed
in
a
single
session
before
any
changes
occurred
in
viewer
count
which
automatically
alters
the
rank
of
the
video
in
the
display
list
and
its
popu-
larity.
Uniform
Resource
Locator
(URL)
addresses
of
videos
were
copied
into
an
excel
sheet
to
form
the
watch
list.
The
final
list
was
overviewed
by
4
assessors
and
a
consensus
was
established
on
the
final
list
according
to
the
exclusion
crite-
ria.
Videos
in
languages
other
than
English,
with
unrelated
content,
or
that
were
shorter
than
1
minute
were
excluded.
Video
lasting
longer
than
15
minutes
were
excluded
because
the
length
of
the
video
may
jeopardize
the
accuracy
of
the
assessment
due
to
the
length.
Questionnaire
1
Q1
had
18
questions
about
the
technique
itself
regarding
safety,
hygiene,
anatomy,
landmarks,
complications,
local
anesthetic
use,
and
equipment.
Each
assessor
gave
a
score
to
each
question
grading
from
1
to
5
(1
being
very
bad
and
5
being
excellent).
Question
10
was
asked
to
determine
nerve-stimulator
usage
and
question
11
and
12
were
exam-
ined
only
for
sole
nerve-stimulator
guided
videos.
In
Q1
the
last
six
questions
were
only
answered
for
ultrasound-guided
blocks
and
they
were
related
to
ultrasound
image,
needle
manipulations,
and
sonographic
image
interpretation.
Ques-
tionnaire
One
(Q1
---
Table
1)
was
prepared
according
to
the
Delphi
method
based
on
the
standard
procedure
definitions
taken
from
the
American
Society
of
Regional
Anesthesia,
and
Miller’s
Anesthesia
textbook.
11,12
The
four
assessors
filled
Q1
for
each
video
individually.
Questionnaire
2
Questionnaire
two
(Q2
---
Table
2),
which
included
14
items
regarding
preparation
and
generic
video
quality
of
each
video,
was
completed
individually.
In
this
second
part,
inves-
tigators
evaluated
the
videos
according
to
the
Guidelines
for
the
Preparation
and
Evaluation
of
Video
Career
Media
by
the
American
National
Career
Development
Association
(NCDA).
13
The
videos
were
marked
from
0
to
5
(where
0
does
not
apply,
1
is
unsatisfactory,
2
is
poor,
3
is
satisfactory,
4
is
good,
and
5
is
outstanding).
The
final
scores
of
each
video
were
averaged
and
grouped
as
follows:
0---13:
unsatisfac-
tory;
14---27:
poor;
28---41:
satisfactory;
42---54:
good;
56---70:
outstanding.
Final
evaluation
meeting
for
disputed
videos
A
consensus
score
was
reached
in
a
focus
group
meeting
for
those
videos
in
which
Fleiss’
Kappa
scores
<
0.20
in
Q1.
The
consultant
anesthesiologist
was
selected
as
moderator
during
the
meeting.
If
ambiguities
could
not
be
reconciled
over
a
video,
‘‘voting’’
was
used
to
reach
a
final
score
for
the
debated
videos.
Statistical
analyses
R
3.4.3
(R
Core
Team;
2017).
Was
used
for
all
data
cleaning,
analysis
and
visualization
processes
and
Inter
Rater
Reliabil-
ity
(IRR)
calculation.
14,15
Agreement
between
assessors
for
each
video
was
defined
according
to
Fleiss’
Kappa
scores:
no
agreement
(<0.20),
insignificant
agreement
(0.0---0.20),
moderate
agreement
(0.21---0.40),
most
part
agreement
(0.41---0.60),
significant
agreement
(0.61---0.80),
and
excel-
lent
agreement
(0.81---1.00).
Results
Video
selection
72
ultrasound-guided
and
14
nerve-stimulator
guided
block
videos,
a
total
of
86
videos
out
of
374
were
evaluated
in
YouTube.
A
total
of
288
videos
were
excluded
for
the
fol-
lowing
reasons:
8
non
English,
288
not
on-topic,
36
repeated
and
16
too
long/short.
The
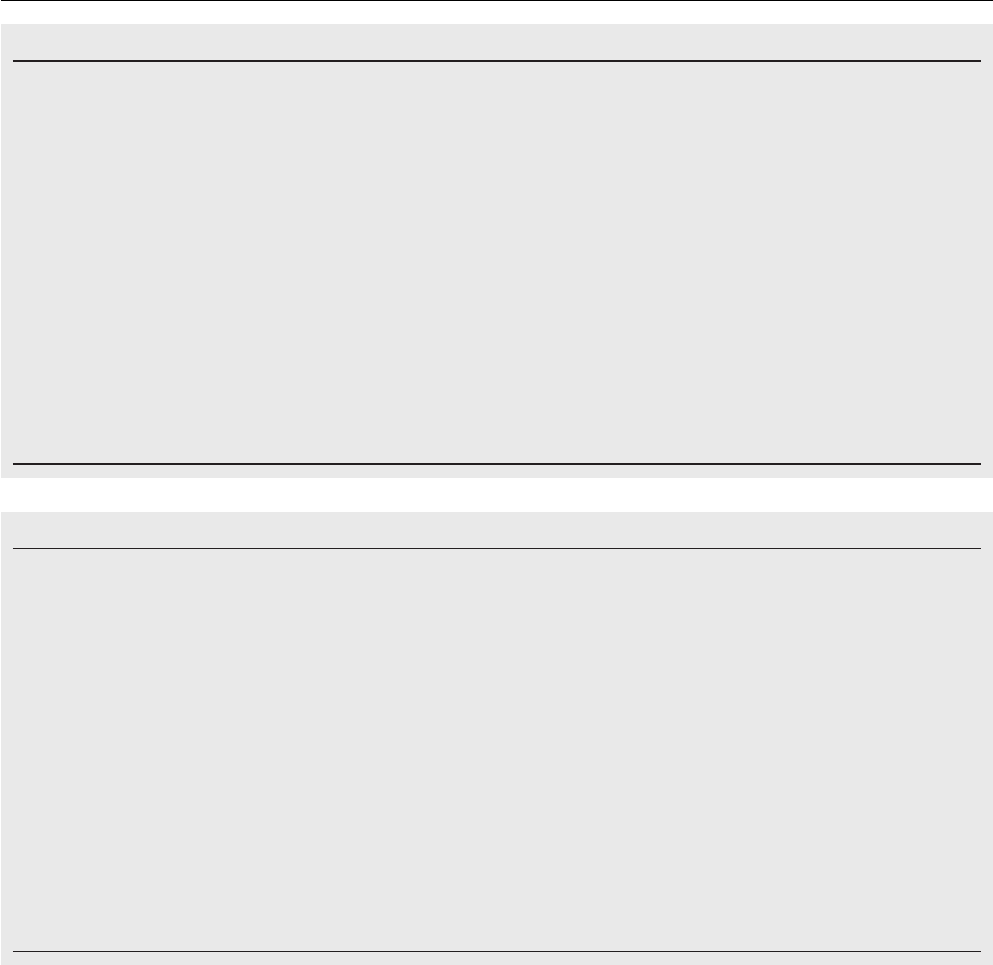
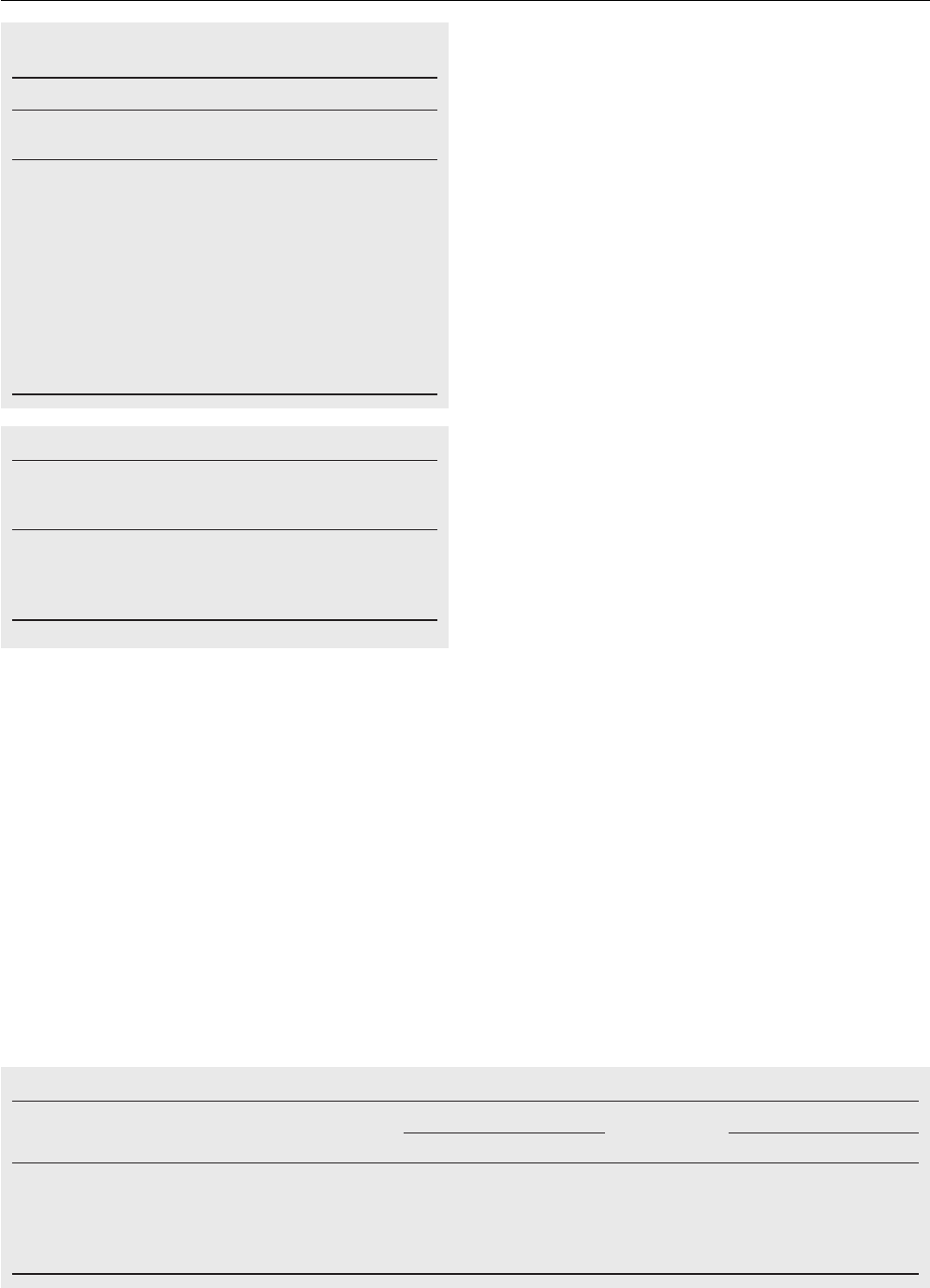
exclusion
criteria
and
numbers
for
the
whole
evaluation
process
can
be
seen
in
Table
3
and
Fig.
1.
Brachial
plexus
videos
in
YouTube
171
Table
1
Questionnaire
1.
Q1
In
which
kind
of
operation
is
this
block
applicable?
Was
this
information
clearly
explained?
Q2
Was
there
clear
explanation
of
the
targeted
skin
dermatomes
innervated
by
the
nerve?
Q3
Were
anatomical
landmarks
clearly
explained
or
marked?
Q4
Were
important
vessels
and
nerve
structures
in
close
relation
to
the
targeted
nerve
clearly
explained?
Q5
Were
possible
complications
related
to
this
block
technique
explained?
Q6
Was
the
information
on
sterilization
procedures
clearly
explained
or
emphasized?
Q7
Was
the
information
about
nerve
stimulator
device
and
needle
choice
clearly
explained?
Q8
Was
the
information
for
skin
local
anesthetic
infiltration
(volume,
name
of
medication)
clearly
explained?
Q9
Was
the
information
about
local
anesthetic
substance
clearly
explained?
Q10
Was
the
nerve
stimulator
used
in
this
block?
Q11
If
YES,
was
the
safe
threshold
level
for
electrical
impulses
clearly
explained?
Q12
If
YES,
were
the
muscle
twitches
regarding
the
stimulated
nerve
clearly
explained?
Q13
Were
the
sono-anatomic
image
recording
and
anatomical
structures
in
the
recording
clear
and
easy
to
perceive?
Q14
Was
the
ultrasound
image
of
the
needle
visible
and
easy
to
follow?
Q15
Were
the
instructions
for
depth,
alignment
and
direction
movements
of
the
needle
clearly
explained?
Q16
Was
the
technical
information
for
probe
selection
and
frequency
regarding
the
ultrasound
device
explained?
Q17
Was
the
information
about
in-plane
or
out-plane
technique
presented
in
the
video?
Q18
Was
the
information
about
the
local
anesthetic
spread
explained?
Table
2
Questionnaire
2.
Q1
Was
the
aim
of
video
clearly
stated
and
was
it
explained
in
the
first
quarter
of
the
video?
Q2
Did
the
title
or
name
of
the
video
match
the
aim
of
the
video?
Q3
Were
the
design
and
the
content
of
the
video
suitable
for
a
targeted
educational
aim?
Q4
Were
the
skills
and
the
technique
of
the
procedure
explained
using
a
standard,
comparable
and
‘‘step
by
step’’
method?
Q5
Was
the
information
given
in
the
video
useful
for
viewers
to
develop/enhance
their
skill
base?
Q6
Was
the
content
of
the
video
appropriate
for
the
health
and
safety
of
both
the
patient
and
the
practitioner?
Q7
Was
the
quality
of
picture
regarding
colors
and
clarity
acceptable?
Q8
Was
the
quality
of
video
sound
acceptable?
(No
sound
should
be
scored
as
zero)
Q9
Was
the
length
of
the
video
in
balance
with
the
content
of
the
video?
Q10
Was
the
information
on
the
date
of
production
or
release,
producers
and
the
references
clearly
explained?
Q11
Were
objectives,
learning
tasks
and
terminology
clearly
stated
in
the
video
enabling
viewers
to
address
those
tasks?
Q12
Did
the
video
have
stop-and-discuss
points,
additional
aids
such
as
scripts
and/or
summarized
information
on
procedure?
Q13
Was
any
information
given
on
a
way
to
evaluate
the
effectiveness
and
reproducibility
of
the
video?
Q14
Did
the
content
of
the
video
stimulate
viewers
to
make
the
transition
from
passive
viewer
to
active
practitioner
in
the
application
of
the
technique?
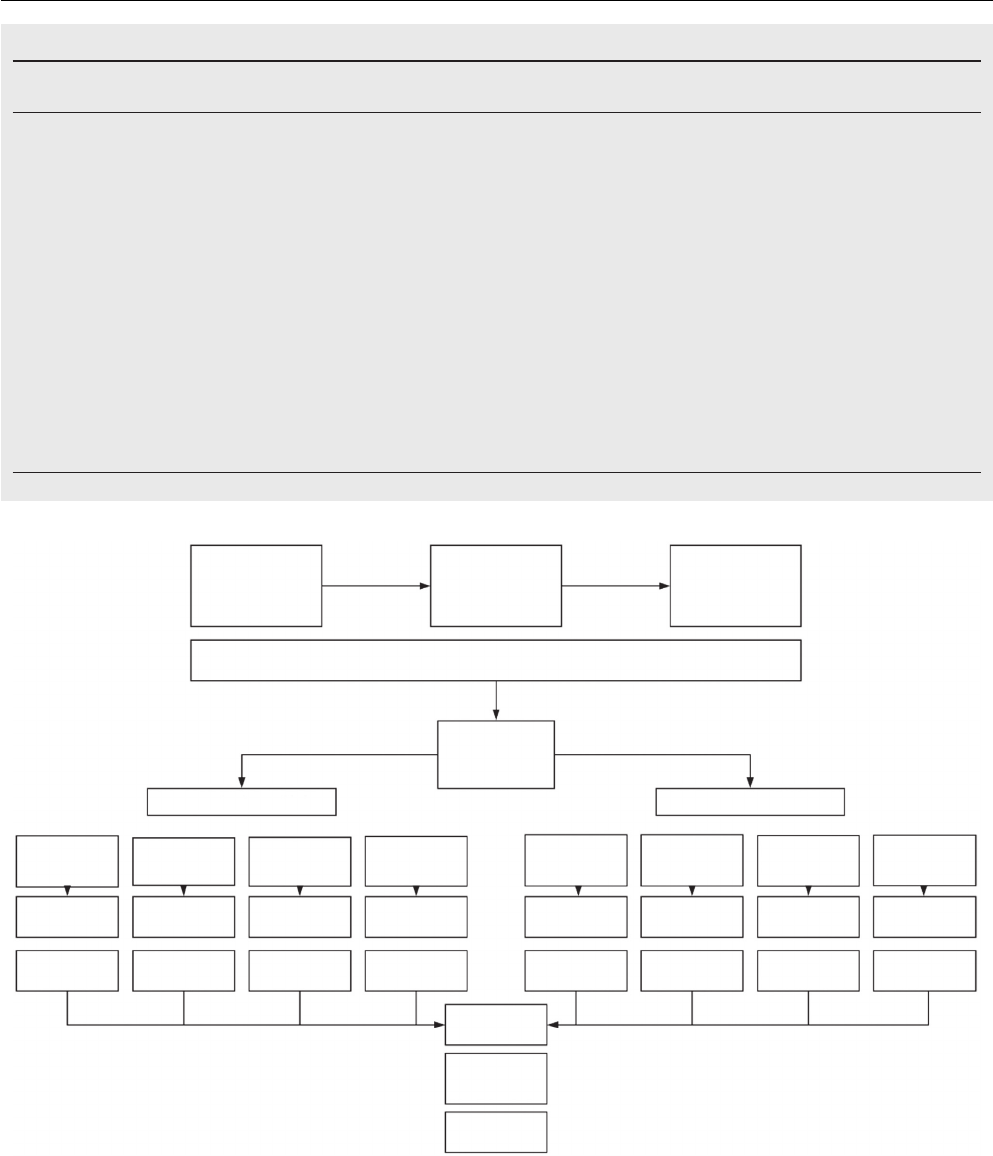
Results
of
Q1
The
final
Q1
scores
for
14
PNS
video
and
72
USG
guided
videos
are
presented
in
Figs.
2
and
3
respectively.
As
can
be
seen
in
the
heat
map
graphics,
the
first
videos
in
every
watch
list
of
each
block
technique
had
greater
scores
than
subsequent
videos
and
the
last
videos
of
the
watch
lists
had
the
lower
scores.
When
we
evaluate
the
average
scores
for
each
ques-
tion
in
Q1,
in
ultrasound-guided
videos
the
least
score
was
1.38
(median
=
3;
25th
percentile
=
1;
75th
per-
centile
=
1)
in
Q1---05
related
to
the
information
on
possible
complications,
and
the
greatest
value
was
3.30
(median
=
3,
25th
percentile
=
2,
75th
percentile
=
5)
in
Q1---13
related
to
sono-anatomy
(Table
4).
For
the
videos
with
nerve
stimulator,
the
lowest
score
was
1.64
(median
=
1;
25th
percentile
=
1;
75th
percentile
=
2)
in
Q1---07,
which
was
related
to
the
nerve
stimulator
device
and
needle
choice,
and
the
highest
was
3.60
(median
=
4,
25th
percentile
=
3,
75th
percentile
=
5)
in
Q1---12
related
to
the
information
on
muscle
twitches
(Table
5).
According
to
the
result
of
question
10
in
Q1,
which
eval-
uates
nerve
stimulator
usage,
in
11
of
72
Ultrasound-guided
videos
nerve-stimulator
was
combined
with
ultrasound
to
demonstrate
muscle
twitches,
however
only
4
videos
had
information
about
lowest
safe
threshold
for
electri-
cal
impulses.
A
total
of
26
videos
were
accompanied
by
a
‘‘written
only’’
explanation
and
seven
videos
provided
no
description
(written
or
verbal)
of
the
procedure
being
undertaken.
Regarding
the
ultrasound-guided
videos,
36
sonographic
recordings
of
successful
interventions
were
shared
and
3
videos
were
animation.
Only
17
videos
referred
to
whether
the
block
was
performed
using
an
out-of-plane
or
in-plane
technique.
172
O.
Selvi
et
al.
Table
3
Video
selection.
Total
number
of
videos
Non-English
Off-Topic
Too
long/
short
Repeated
videos
Selected
videos
Interscalene
B.
(Nerve
Stimulator
guided)
31
1
25
1
1
3
Interscalene
B.
(Ultrasound
guided)
41
2
13
4
1
21
Supraclavicular
B.
(Nerve
Stimulator
guided)
34
1
28
0
1
4
Supraclavicular
B.
(Ultrasound
guided)
65
3
37
2
3
20
Infraclavicular
B.
(Nerve
Stimulator
guided)
37
1
27
1
7
1
Infraclavicular
B.
(Ultrasound
guided)
60
0
29
1
15
15
Axillary
B.
(Nerve
Stimulator
guided)
20
0
13
1
0
6
Axillary
B.
(Ultrasound
guided)
86
0
56
6
8
16
B.,
block.
Selection of brachial
plexus bloc
ks
Selection of the
final watching list of
the videos
Final videos n:86
Data analysis
Final e
valuation
meeting for
debated videos
n:21
n:20
n:15
n:16n:6n:1n:4
28 excluded
Interscalene
block videos
n:31
Interscalene
block videos
n:41
Supraclavicular
block videos
n:34
Supraclavicular
block videos
n:65
Infraclavicular
block videos
n:37
Axillary ner
ve
block videos
n:20
Axillary ner
ve
block videos
n:86
Infraclavicular
block videos
n:60
30 excluded
36 excluded
14 excluded
20 excluded
45 excluded
45 excluded
70 excluded
n:3
Nerve stimulator guided
Ultrasound guided
Assessors team:1 consultant and 3 experienced anesthesiologist
06.10.2017 search f
or
videos with key words
in youTube
Total 374 videos
Figure
1
Flow
chart
of
the
study.
In
Q1
Ultrasound-guided
interscalene
videos
had
higher
scores
compared
to
the
other
ultrasound-guided
blocks.
Ultrasound-guided
axillary
blocks
had
lowest
scores
in
Q1.
Videos
of
axillary
blocks
with
nerve
stimulator
had
highest
scores
however,
supraclavicular
blocks
with
nerve
stimulator
had
the
lowest
average
scores
in
Q1
(Table
6).
IRR
was
examined
for
Q1,
Kappa
score
was
between
0.81
and
1.00
for
28
videos
(excellent
agreement),
0.61---0.80
(significant
agreement)
for
8
videos,
0.41---0.60
(most
part
agreement)
for
32
videos
and
0.21---0.40
(moderate
agree-
ment)
for
18
videos.
The
greatest
and
least
Kappa
scores
were
1.00
and
0.23
respectively
for
Q1.
Ten
videos
were

Brachial
plexus
videos
in
YouTube
173
12
11
09
08
07
06
05
04
03
02
01
12 13 1410 110908070605
Video
Question
Average score
Videos 1-3 Interscalane, 4-7 Supraclavicular, 8 Infraklavicular, 9-14 Axillary
0
1
2
3
4
5
04030201
Figure
2
Distribution
of
scores
for
the
brachial
plexus
nerve
block
videos
performed
with
nerve
stimulator.
scored
as
‘unsatisfactory’
for
all
questions
resulting
in
Kappa
scores
of
1.0
for
these
videos.
Results
of
Q2
The
results
of
Q2,
which
reflects
the
preparation
and
generic
video
quality
of
videos
as
educational
material,
can
be
seen
Table
4
Question
based
evaluation
of
the
scores
for
ultra-
sound
guided
brachial
plexus
block
videos
in
Q1.
USG
video
scores
by
question
Question
25th
percentile
Mean
Median
75th
percentile
Q13
2
3.3
3
5
Q04
2
3.03
3
5
Q03
1
2.7
3
4
Q14
1
2.7 3
4
Q18
1
2.6 2
4
Q15
1
2.6 2
4
Q17
1
2.4
2
4
Q01
1
1.9
1
2
Q16
1
1.8
1
2
Q08
1
1.8
1
2
Q07
1
1.6 1
2
Q06
1
1.6 1
1
Q02
1
1.5 1
1
Q09
1
1.4 1
1
Q05
1
1.4 1
1
in
Table
7,
with
65.3%
of
Ultrasound-guided
videos
and
42.8%
of
blocks
with
nerve-stimulator
having
worse
than
satisfac-
tory
scores.
Only
5
Ultrasound-guided
videos
and
1
classical
nerve
block
video
had
outstanding
results.
Video
Average score
0
1
2
3
4
5
Question
Interscalene videos
Supraclavicular videos
Inf
raclavicular videos
Axillary videos
14
15
16
17
18
13
09
08
07
06
05
04
03
02
01
14
15
16
17
18
13
09
08
07
06
05
04
03
02
01
14
15
16
17
18
13
09
08
07
06
05
04
03
02
01
14
15
16
17
18
13
09
08
07
06
05
04
03
02
01
14 15 16 17 18 19 20 21
22
57
42 43 44 45 46 47 48
49
50
51 52
53 54 55 56
58
59 60 61 62 63
64
65 66 67 68 69
70
71 72
23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41
1309 10 11 120807060504030201
Figure
3
Distribution
of
scores
for
the
ultrasound
guided
brachial
plexus
nerve
block
videos.
174
O.
Selvi
et
al.
Table
5
Question
based
evaluation
of
the
scores
for
nerve
stimulator
guided
brachial
plexus
block
videos
in
Q1.
NS
video
scores
by
question
Question
25th
percentile
Mean
Median
75th
percentile
Q12
3
3.6
4
5
Q03
2
3.1 3
4
Q11
2
3.1 3
4
Q01
1
2.5 2
4
Q08
1
2.4
3
3
Q02
1
2.3
2
4
Q09
1
2.3
2
3.25
Q04
1
2.3
2
3.25
Q06
1
2.0
2
2
Q05
1
1.6
1
2
Q07
1
1.6
1
2
Table
6
Mean
scores
of
the
videos
in
Q1.
Mean
score
for
nerve
stimulator
videos
Mean
score
for
ultrasound
videos
Axillary
B.
2.57
1.84
Infraclavicular
B.
3.11
1.86
Interscalene
B.
2.81
2.51
Supraclavicular
B.
1.82
2.25
B.,
blocks.
Discussion
Since
the
core
aspect
of
ultrasound-guided
nerve
block
education
is
‘‘visual’’
in
nature,
using
videos
for
regional
anesthesia
education
can
be
crucially
beneficial
for
trainees.
How
to
produce
reliable
visual
materials
and
incorporate
them
into
regional
anesthesia
education
is,
in
itself,
an
important
issue
for
medical
practice.
Therefore,
there
do
exist
regional
anesthesia
videos
which
have
been
created
by
professional
institutions
with
high
accuracy,
quality
and
credibility
for
use
in
regional
anesthesia
train-
ing,
requiring
extensive
planning
and
careful
execution.
As
a
complementary
part
of
this
visual
guidance
recording
regional
anesthesia
interventions
and
using
them
to
recre-
ate
visual
feedback
videos
can
also
be
extremely
useful
for
self-assessments
in
regional
anesthesia
education.
Even
the
qualified
residents
in
regional
anesthesia
can
use
any
of
these
videos
as
a
source
of
information
when
they
lose
familiarity
with
a
specific
regional
anesthesia
block
tech-
nique
but
still
have
to
proceed
with
the
technique.
7,8,16---18
According
to
the
results
of
the
current
study,
the
most
rated
videos
were
prepared
by
professional
institutions,
and
in
these
videos
the
sonographic
image
and
position-
ing
of
ultrasound
probe
shared
the
same
screen
so
that
the
viewer
can
observe
the
relationship
between
the
align-
ment,
tilting,
pressure
and
rotation
maneuvers
related
to
the
USG
view.
These
most
highly
rated
videos
included
many
of
the
aspects
recommended
by
the
new
basic
simulation
assessment
tool.
This
tool
promised
to
improve
the
nec-
essary
skills
for
successful
Needle
Insertion
Accuracy
(NIA)
for
ultrasound-guided
nerve
blocks,
such
as
‘‘approach’’,
‘‘alignment’’,
‘‘movement’’,
‘‘location’’
and
‘‘targeting’’.
All
these
skills
require
dimensional
thinking,
interpretation
of
a
two
dimensional
screen
and
hand---eye
coordination.
Basically
this
new
visual
and
video
based
regional
anes-
thesia
training
device
emphasizes
the
value
of
screening
both
the
hand
position
and
the
ultrasound
image
simulta-
neously
on
the
same
screen.
7
Thus,
while
creating
visual
educational
materials
for
ultrasound-guided
regional
anes-
thesia
blocks,
this
technical
approach
can
empower
the
value
of
the
videos.
These
videos
which
are
systematic
in
their
approach
need
to
demonstrate
target
nerve
location,
direction
of
needle
toward
the
target
nerve
and
the
correct
method
of
administering
the
local
anesthetic
to
the
target
area.
Regulations
over
patient
safety
and
quality
standards
have
brought
new
issues
for
regional
anesthesia
education.
19
To
overcome
these
difficulties
in
regional
block
education,
simulation
based
training
methods
have
been
described
in
recent
years
which
allow
trainees
to
gain
skills
such
as
rotation,
alignment,
tilting
and
targeting
before
they
practice
on
real
patients.
20
It
has
been
shown
that
these
sonographic
skills
were
performed
more
successfully
by
anesthesia
trainees
when
they
were
provided
with
expert-
guided
feedback.
21
Although
we
do
not
recommend
YouTube
videos
as
a
learning
tool
as
per
our
findings,
publishing
recor-
dings
of
these
modern
regional
anesthesia
training
videos
together
with
explanatory
feedback
points
may
help
watch-
ers
to
understand
the
steps
and
errors
made
by
trainees.
These
videos
when
made
by
reputable
medical
institutes
might
be
quite
beneficial
for
regional
anesthesia
trainees
or
residents.
They
may
refresh
their
knowledge
regarding
ultrasound-guided
nerve
blocks
simply
by
watching
easily
available
YouTube
videos.
Addition
to
this,
institutes
and
their
followers
can
easily
meet
in
YouTube’s
social
platform
with
the
help
of
these
high-quality
education
videos.
Thus,
Table
7
Preparation
and
generic
video
quality
of
the
videos
(Q2).
Evaluation
Score
USG
videos
NS
videos
n
Percent
n
Percent
Unsatisfactory
0---13
19
26.4
1
7.1
Poor
14---27
28
38.9
5
35.7
Satisfactory
28---41
11
15.3
5
35.7
Good
42---54
9
12.5
2
14.3
Outstanding
56---70
5
6.9
1
7.1

Brachial
plexus
videos
in
YouTube
175
regional
anesthesia
applicants
may
meet
and
interact
in
an
alternative
widely-used
platform
to
share
and
expand
their
experiences.
The
safety
standard
of
procedure
application
in
the
videos
was
ambiguous
too.
In
ultrasound-guided
videos
the
lowest
average
score
was
in
question
5
which
asks
the
level
of
information
on
possible
complications
of
the
blocks,
and
this
fact
downgrades
the
reliability
of
videos
in
terms
of
safety.
Among
these
same
videos,
19
were
without
a
sound
recording,
relying
on
written
instructions
and
signs
to
deliver
the
presentation
and
therefore
failing
to
give
adequate
information
on
equipment,
preparation,
drug
doses,
patient
positioning,
and
sterilization.
They
are
a
contingent
part
of
the
apprenticeship
style
training
method,
a
type
of
educa-
tional
approach
that
can
be
found
responsible
to
prevent
regional
anesthesia
residents
from
receiving
standardized
education.
19
Unfortunately,
short
videos
were
unable
to
score
well
on
a
majority
of
Q1
and
Q2
questions.
Only
6
of
a
total
of
86
videos
got
outstanding
quality
scores
and
the
length
of
these
videos
were
over
seven
minutes.
Therefore,
it
can
be
postulated
that
any
visual
education
material
prepared
for
regional
anesthesia
education
should
not
be
too
short.
Although
some
short
videos
contain
valuable
information
and
tips,
they
are
often
difficult
to
understand
for
some-
one
who
is
new
to
the
technique.
Furthermore,
in
similar
future
studies
based
on
visual
material
analysis,
a
longer
‘‘minimum
time
limit’’
can
be
applied
as
exclusion
criteria
depending
on
the
targeted
outcome.
The
final
questions
of
the
Q2
assessment,
regarding
whether
or
not
the
videos
possessed
the
necessary
detail
for
accurate
re-enactment
of
the
procedure
in
a
clinical
set-
ting,
received
the
lowest
scores
from
the
assessors.
Only
two
videos
received
full
points
from
Q2.
Again
this
confirms
that
YouTube
videos
have
poor
overall
preparation
and
could
be
inadequate
as
refresher
material
for
the
selected
four
upper
body
peripheral
nerve
block
interventions.
According
to
the
results
of
this
study,
there
were
five
times
more
ultrasound-guided
BPNB
videos
on
YouTube
than
those
proceeding
with
conventional
nerve
stimulators
among
the
videos
examined
for
this
study.
This
shows
the
increasing
tendency
for
performing
ultrasound
guided
nerve
blocks
and
also
indicates
the
level
of
demand
for
them
as
learning/sharing
tools
on
social
platforms.
Health
institu-
tions,
universities
or
regional
anesthesia
associations
may
contribute
to
the
spread
of
more
accountable
and
credible
videos
on
YouTube
for
regional
anesthesia
which
priori-
tize
patient
safety
over
commercial
concerns,
such
that
commercial
institutions
and
individual
health
providers
may
be
inspired
by
the
setup
of
these
videos
to
reproduce
similar
high
quality
videos.
Thus
the
overall
quality
of
regional
anes-
thesia
videos
on
YouTube,
a
platform
of
great
public
impact
and
popularity,
may
provide
more
accurate
and
trustworthy
information.
Limitations
The
limitations
of
this
study
should
be
considered
while
reviewing
our
data.
First,
each
assessor
viewed
the
selected
videos
in
the
same
order
according
to
the
pre-determined
watch
list
---
ideally
the
assessors
could
have
reviewed
the
videos
in
random
order.
Although
assessors
watched
videos
independently,
video
randomization
would
have
prevented
the
repeated
effect
of
one
video
on
the
judgment
of
the
next
from
distorting
results.
Finally,
we
did
not
examine
num-
bers
of
viewers
for
each
video,
which
might
be
seen
as
a
good
predictor
for
the
quality
and
‘‘disseminative
impact’’
of
the
video.
22
However,
former
studies
have
revealed
no
correlation
between
the
quality
of
videos
and
views/month
and
this
fact
dissuaded
us
from
analyzing
data
on
viewer
counts.
6,9
Conclusion
The
utility,
scientific
rigor
and
accountability
of
BPNB
videos
in
YouTube
does
not
correlate
with
YouTube’s
modernity
and
mass
availability.
The
majority
of
the
videos
lack
the
sys-
tematic
approach
necessary
to
safely
guide
someone
seeking
information
about
the
BPNB
examined
for
this
study.
If
pro-
fessional
institutions
and
universities
publish
more
videos
with
predefined
competencies
on
social
media
platforms
like
YouTube,
they
may
present
a
good
example
for
safe
and
successful
interventions.
Conflicts
of
interest
The
authors
declare
no
conflicts
of
interest.
Acknowledgments
The
authors
would
like
to
thank
Dr.
George
Shorten,
member
of
Department
of
Anesthesiology
and
Intensive
Care,
Uni-
versity
Collage
Cork,
for
his
valuable
contributions
to
this
study.
References
1.
Knight
E,
Intzandt
B,
MacDougall
A,
et
al.
Information
seeking
in
social
media:
a
review
of
youtube
for
sedentary
behavior
content.
Interact
J
Med
Res.
2015;4:e3.
2.
Azer
SA,
Algrain
HA,
AlKhelaif
RA,
et
al.
Evaluation
of
the
edu-
cational
value
of
YouTube
videos
about
physical
examination
of
the
cardiovascular
and
respiratory
systems.
J
Med
Internet
Res.
2013;15:e241.
3.
Romanov
K,
Nevgi
A.
Do
medical
students
watch
video
clips
in
eLearning
and
do
these
facilitate
learning?
Med
Teach.
2007;29:484---8.
4.
Mathis
S,
Schlafer
O,
Abram
J,
et
al.
Anesthesia
for
medi-
cal
students:
a
brief
guide
to
practical
anesthesia
in
adults
with
a
web-based
video
illustration.
Anaesthesist.
2016;65:
929---39.
5.
DelSignore
LA,
Wolbrink
TA,
Zurakowski
D,
et
al.
Test-enhanced
E-learning
strategies
in
postgraduate
medical
education:
a
ran-
domized
cohort
study.
J
Med
Internet
Res.
2016;18:e299.
6.
Tackett
S,
Slinn
K,
Marshall
T,
et
al.
Medical
education
videos
for
the
world:
an
analysis
of
viewing
patterns
for
a
YouTube
channel.
Acad
Med.
2018;93:1150---6.
7.
Das
Adhikary
S,
Karanzalis
D,
Liu
WR,
et
al.
A
prospec-
tive
randomized
study
to
evaluate
a
new
learning
tool
for
ultrasound-guided
regional
anesthesia.
Pain
Med.
2017;18:
856---65.
8.
Godwin
HT,
Khan
M,
Yellowlees
P.
The
educational
potential
of
YouTube.
Acad
Psychiatry.
2017;41:823---7.

176
O.
Selvi
et
al.
9.
Tulgar
S,
Selvi
O,
Serifsoy
TE,
et
al.
YouTube
as
an
infor-
mation
source
of
spinal
anesthesia,
epidural
anesthesia
and
combined
spinal
and
epidural
anesthesia.
Rev
Bras
Anestesiol.
2017;67:493---9.
10.
Rössler
B,
Lahner
D,
Schebesta
K,
et
al.
Medical
information
on
the
Internet:
quality
assessment
of
lumbar
puncture
and
neuroaxial
block
techniques
on
YouTube.
Clin
Neurol
Neurosurg.
2012;114:655---8.
11.
Americana
Society
of
Regional
Anesthesia
and
Pain
Medicine.
Available
at:
https://www.asra.com/pain-
resource/category/9/upper-extremity-blocks.
12.
Miller
RD.
Miller’s
anesthesia.
7th
ed.
Philadelphia:
Else-
vier/Churchill
Livingstone;
2010.
p.
1639---703.
13.
National
Career
Development
Association
(NCDA)
Guide-
lines
for
the
Preparation
and
Evaluation
of
Video
Career
Media.
Available
at:
https://www.ncda.org/aws/NCDA/
asset
manager/get
file/3401
[accessed
17
May
2017].
14.
R
Core
Team
(2017).
R:
A
language
and
environment
for
statisti-
cal
computing.
R
Foundation
for
Statistical
Computing,
Vienna,
Austria.
https://www.R-project.org/
[accessed
3
July
2017].
15.
Matthias
Gamer,
Jim
Lemon
and
Ian
Fellows
Puspendra
Singh
(2012).
irr:
Various
Coefficients
of
Interrater
Reliability
and
Agreement.
R
package
version
0.84.
https://CRAN.R-project.
org/package=irr
[accessed
3
July
2017].
16.
Pedersen
K,
Moeller
MH,
Paltved
C,
et
al.
Students’
learning
experiences
from
didactic
teaching
sessions
including
patient
case
examples
as
either
text
or
video:
a
qualitative
study.
Acad
Psychiatry.
2018;42:622---9.
17.
Sainsbury
JE,
Telgarsky
B,
Parotto
M,
et
al.
The
effect
of
ver-
bal
and
video
feedback
on
learning
direct
laryngoscopy
among
novice
laryngoscopists:
a
randomized
pilot
study.
Can
J
Anaesth.
2017;64:252---9.
18.
Beard
HR,
Marquez-Lara
AJ,
Hamid
KS.
Using
wearable
video
technology
to
build
a
point-of-view
surgical
education
library.
JAMA
Surg.
2016;151:771---2.
19.
Smith
HM,
Kopp
SL,
Jacob
AK,
et
al.
Designing
and
implementing
a
comprehensive
learner-centered
regional
anesthesia
curricu-
lum.
Reg
Anesth
Pain
Med.
2009;34:88---94.
20.
Adhikary
SD,
Hadzic
A,
McQuillan
PM.
Simulator
for
teaching
hand---eye
coordination
during
ultrasound-guided
regional
anes-
thesia.
Br
J
Anaesth.
2013;111:844---5.
21.
Ahmed
OMA,
Niessen
T,
O’Donnell
BD,
et
al.
The
effect
of
metrics-based
feedback
on
acquisition
of
sonographic
skills
rel-
evant
to
performance
of
ultrasound-guided
axillary
brachial
plexus
block.
Anesthesia.
2017;72:1117---24.
22.
Trueger
NS,
Thoma
B,
Hsu
CH,
et
al.
The
altmetric
score:
a
new
measure
for
article-level
dissemination
and
impact.
Ann
Emerg
Med.
2015;66:549---53.
